PREAMBLE
This paper is a summary of analysis of ONS data undertaken
since the pandemic hit the UK in March 2020. It was designed to analyse
variations in COVID-19 deaths at the level of small geographical areas and link
them to other data on those areas, particularly deprivation and ethnicity. We
first present the national picture.
NATIONAL
ONS published the weekly level death statistics on 14 July
enabling a comparison of COVID-19 deaths and excess deaths up to week 27 (3
July 2020). Figure 1 summarises this data. Excess deaths are calculated as the
difference between all deaths that occurred in that week averaged over the last
five years and the actual number of deaths in that week this year. It is
thought to be a safer estimate of COVID-19-related deaths because not all
deaths, perhaps particularly in the first weeks of pandemic, were recorded as
COVID-19- related. The Figure shows the sharp increase in deaths beginning in
week 12 around the 20 March. Thankfully there has been a sharp reduction in
COVID-19-registered and excess deaths since week 16 around 17 April. It is also
interesting that the excess deaths have begun to mirror much more closely the
COVID-19 deaths.
COVID-19 DEATHS, DEPRIVATION and ETHNICITY
ONS itself has published many interesting analyses of
COVID-19 deaths, which have shown higher numbers of deaths by the level of area
deprivation, and higher levels of deaths among BAME people.[1]
[2]
[3]
Platt and Warwick[4] found that some ethnic groups have higher rates
of COVID-19 mortality even though on the basis of their age they should have
lower death rates. After accounting for the effects of age and geography the Black
Caribbean group have deaths three times higher than the White British. There
has been one ONS study that has linked death certificates mentioning COVID-19
with Census data on age, sex, ethnicity, other demographic characteristics and
socio-economic status including the Index of Deprivation decile. They found
that males and females of Black ethnicity were 1.9 times more likely to die
than those of White ethnicity and men of Bangladeshi and Pakistani origin were 1.8
times and females 1.6 times more likely to die than those of White ethnicity.[5]
However the analysis was undertaken at local authority level.
The figure below, based on the latest ONS deaths data for
England published by ONS on 12 May, indicate that the age standardised death
rates from COVID-19 are more than twice as high in the most deprived deciles as
they are in the least. But there is very little difference in COVID-19 deaths
as a proportion of all deaths by deprivation.
Figure 2. Age standardised Covid deaths in England by IMD
decile.[9]
AT LOCAL AUTHORITY LEVEL
Meanwhile, ONS published new data by Local Authority, which
we have analysed to explore variations in deaths by deprivation and ethnicity.[1]
Method
We created a new data set by merging the ONS data on all
deaths and COVID-19 deaths up to the end of May with Index of Deprivation data
by local authority and estimates of the ethnic mix of the population produced
by ONS in 2016. We produced two dependent variables: the age-standardised death
rate due to COVID-19 and the age-standardised deaths from COVID-19 as
percentage of all age-standardised deaths.
Results
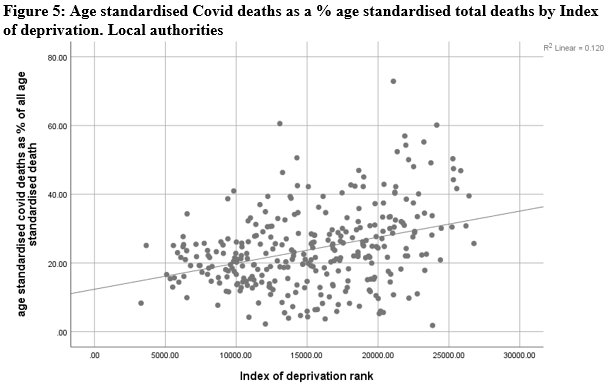
Firstly, we show the bivariate relationship between our two
dependent variables and deprivation and BAME in the following scatterplots. It
can be seen that for both dependent variables there is a stronger association
with BAME than there is with deprivation.
[1] ONS Number
of deaths and age-standardised rates, by sex, Local Authorities in England and
Wales, deaths occurring between March and May 2020
Then in the tables below we present the results of two
regressions with our dependent variables.
In Table 1 the higher the % BAME the more COVID-19 deaths as
% of the population. The index of deprivation rank makes little contribution
and the more deprived the LA the lower the deaths. Using age-standardised COVID-19 deaths as a
percentage of all age-standardised deaths as our dependent variable, the ID
rank is significant and negative – the more deprived an area the higher the
COVID-19 deaths after controlling for BAME.
Table
1: Regression of age-standardised COVID-19 deaths by ID and BAME, local
authority level
|
Age-standardised COVID-19 death rate
|
Age-standardised COVID-19 deaths as a
percentage of all age-standardised deaths
|
|
|
β
|
β
|
|
|
Index of deprivation rank
|
0.104 (p=0.015)
|
0.132 (p=0.004)
|
|
Percentage of the population who are
BAME
|
0.673 (p<0.001)
|
0.621 (p<0.001)
|
|
R-squared
|
0.51
|
0.46
|
We
repeated this analysis to check whether there was a London effect independent
of ethnicity and deprivation. We found that once a London dummy had been
introduced the age-standardised COVID-19 death rate was still almost entirely
explained by ethnicity, London was not significant; for age-standardised
COVID-19 deaths as a % of all age-standardised deaths London was a significant
factor but the main explanatory factor was still ethnicity.
The problem with this analysis is that local authorities are
really too large spatial entities to analyse the impact of ethnicity and
deprivation where variation within the area may be higher than variation
between the area. So, we repeat the analysis at smaller area level.
AT SMALL AREA LEVEL
We also attempt to analyse COVID-19 deaths by deprivation
and ethnicity at small area level. One other justification for making an
attempt to analyse COVID-19 deaths at small area level is that although it is
analysis at spatial rather than individual level, there are doubts about the
accuracy of ethnic group registration in hospital episodes statistics.
Method
The measure of deprivation used is the Index of Deprivation
(IMD) 2019. This is derived from the weighted average of seven domains of
deprivation: income, employment,
education, health, crime, barriers (to housing and services) and living
environment. Each of these is the product themselves of a number of indicators.
The ID domains are first derived for 32,844 Lower-layer Super Output areas (LSOA).
The ONS has combined deaths from COVID-19 and other causes into Middle Level
Super Output Areas (MSOA) with an average population of 8243 in England - on
the grounds that the number of deaths is too low to analyse at the LSOA level.
We extracted the ranks for the Index of Deprivation by LSOA
and summarised them into MSOAs using the ONS look-up tables. The lower the rank
the more deprived.
We then added one other indicator to the data set: the % of the
population who are Black, Asian, Mixed ethnic group (BAME) all at MSOA level - all derived by ONS from 2011 census data.[1]
This means that these data are not up to date.
We use two dependent variables: COVID-19 deaths as a
percentage of all deaths March to May in each MSOA; COVID-19 deaths per 1000 of the population in
each MSOA. The latter standardises the results to control for variation in the
populations sizes of MSOAs (which are quite large – ranging from 2,242-24,969. These
are for the period from the beginning of March to the end of May published by
ONS on 12 June 2020.[2]
It proved impossible to age-standardise the death rates at MSOA level because
there are too few cases. So, in the regressions we include age covariates to
see the effect of IMD and ethnicity, after controlling for age. After looking
at the death rates by age group we used six groups, under 40, 40-59, 50-59,
60-69, 70-79 and 80+. So, we include the number in the population of each MSOA for each of those age
groups. We are not interested in the estimates of these parameters, just the
fact they control for the age structure of each MSOA population.
Results
Bivariate associations are summarised in Table 2, showing that
the lower the IMD, that is the more deprived the area, the higher the COVID-19 deaths,
and the higher the proportion of BAME the higher the deaths. The associations
are stronger for BAME than for the IMD.
Table 2: Correlation matrix
|
Correlations
|
|||||
|
|
Proportion of all deaths which are COVID
|
Covid deaths per 1000 of the population
|
% BAME
|
IMDrank
|
|
|
Proportion of all deaths which are COVID-19
|
Pearson Correlation
|
1
|
.699**
|
.424**
|
-.113**
|
|
Sig. (2-tailed)
|
|
<0.001
|
<0.001
|
<0.001
|
|
|
N
|
6791
|
6791
|
6791
|
6791
|
|
|
COVID-19 deaths per 1000 of the population
|
Pearson Correlation
|
0.699**
|
1
|
0.094**
|
-0.060**
|
|
Sig. (2-tailed)
|
<0.001
|
|
<0.001
|
<0.001
|
|
|
N
|
6791
|
6791
|
6791
|
6791
|
|
|
% BAME
|
Pearson Correlation
|
0.424**
|
0.094**
|
1
|
-0.342**
|
|
Sig. (2-tailed)
|
<0.001
|
<0.001
|
|
<0.001
|
|
|
N
|
6791
|
6791
|
6791
|
6791
|
|
|
IMD rank
|
Pearson Correlation
|
-0.113**
|
-0.060**
|
-0.342**
|
1
|
|
Sig. (2-tailed)
|
<0.001
|
<0.001
|
<0.001
|
|
|
|
N
|
6791
|
6791
|
6791
|
6791
|
|
|
**. Correlation is significant at the 0.01
level (2-tailed).
|
|||||
As before, we summarise the results in the form of simple regressions
for each dependant variable.
Table
3 column 1-2 shows the regression of COVID-19 deaths as a % of all deaths. Here
BAME contributes much more to the variation than IMD. Indeed, the latter is not
significant. As there is some risk of collinearity in that BAME and IMD are weakly
correlated (r=-0.342) we introduce an interaction variable. Columns 3-4 include
an interaction effects, with the same findings. This model explains 20.5% of
the variation.
|
|
COVID-19
deaths as a % of all deaths including IMD and % BAME adjusted for age
|
COVID-19
deaths as a % of all deaths including IMD and % BAME adjusted for age with
BAME and IMD interaction
|
COVID-19
deaths per 1000 of the population including IMD rank and % BAME
|
COVID-19
deaths per 1000 of the population including IMD rank and % BAME and
interaction
|
||||
|
|
β
|
p
|
β
|
p
|
β
|
p
|
β
|
p
|
|
Age_Under40
|
-0.132
|
<0.001
|
-0.135
|
<0.001
|
-0.229
|
<0.001
|
-0.23
|
<0.001
|
|
Age40_49
|
0.087
|
<0.001
|
0.08
|
0.001
|
0.024
|
0.365
|
0.02
|
0.457
|
|
Age50_59
|
0.167
|
<0.001
|
0.175
|
<0.001
|
0.126
|
<0.001
|
0.131
|
<0.001
|
|
Age60_69
|
-0.216
|
<0.001
|
-0.241
|
<0.001
|
-0.142
|
<0.001
|
-0.157
|
<0.001
|
|
Age70_79
|
-0.098
|
0.013
|
-0.044
|
0.271
|
-0.342
|
<0.001
|
-0.311
|
<0.001
|
|
Age_80plus
|
0.064
|
0.005
|
0.048
|
0.035
|
0.534
|
<0.001
|
0.524
|
<0.001
|
|
IMD rank
|
0.018
|
0.178
|
-0.055
|
0.001
|
-0.135
|
<0.001
|
-0.176
|
<0.001
|
|
% BAME
|
0.393
|
<0.001
|
0.262
|
<0.001
|
0.166
|
<0.001
|
0.092
|
<0.001
|
|
Interaction between IMD and % BAME
|
0.164
|
<0.001
|
|
|
0.093
|
<0.001
|
||
|
|
Columns 5-6 show the results for COVID-19 deaths
per 1000 of the population in each MSOA. Again, BAME has a slightly stronger
effect than IMD rank. The proportion of variation explained by this model is
10.9%. When the interaction effect is added in Columns 7-8, the IMD becomes a
more important determinant than BAME of variation in COVID-19 deaths per 1000.
Discussion
The overall impression from this analysis is that ethnicity
and deprivation both contribute to increasing the chances of dying of COVID-19,
but ethnicity explains more variation than IMD on most models.
This is, frankly, quite a surprise – especially given the
clear association between deprivation and health inequalities. It is beyond the
scope of this paper to explain it, but there a number of possibilities
discussed by other research teams, for example see an summary here.
All this needs further research.





No comments:
Post a Comment